How to check client eligibility in ABA Matrix (for administrative staff)
This guide offers essential insights on how to efficiently check client eligibility through ABA Matrix, ensuring accurate insurance coverage verification before service delivery. It highlights multiple methods for checking eligibility, including features for adding new payers and tracking historical eligibility checks. By following these steps, you can enhance billing accuracy and minimize claim issues, ultimately improving service management and client satisfaction.
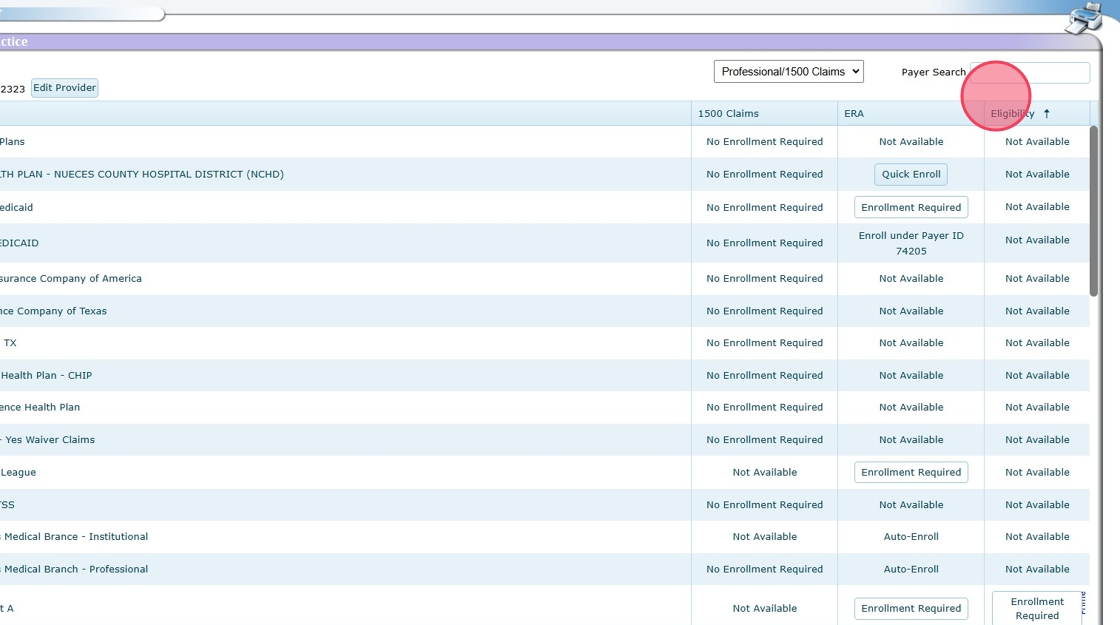
Verify Eligibility Enrollment in ClaimMD
Before running eligibility checks in ABA Matrix, ensure that you have completed eligibility enrollment in ClaimMD for the insurance providers you are working with.
- Eligibility enrollment must be completed for any payers you wish to check benefits and eligibility for.
- If eligibility is not enabled for a specific payer, the system will not be able to retrieve coverage information.
Additionally, note that eligibility requests may be subject to limits based on your ClaimMD account type:
- ClaimMD Unlimited Account – Includes 1,000 eligibility requests per month.
- ClaimMD Small Volume Account – Includes 100 eligibility requests per month; additional requests are billed at $0.50 each.
- ClaimMD Basic Account – No included eligibility requests; each request is billed at $0.30.
🚀 In most cases, enrollment is Quick Enroll, allowing you to complete it instantly with just one click, no waiting required!
1. To activate eligibility for any payers you want to check benefits and eligibility for, go to the Provider Enrollment section

2. The Eligibility column will give you instructions to activate eligibility.
- Not Available: This means that eligibility verification is not supported for the selected payer through ClaimMD. You will need to check eligibility directly with the payer outside of ClaimMD.
- Quick Enroll: This option allows for eligibility verification without requiring a formal enrollment process. Providers can start checking patient eligibility when their ClaimMD account is set up, they just have to click the quick enroll option.
- Enrollment Required: For some payers, a formal enrollment process is needed before eligibility checks can be performed. This involves submitting an enrollment request through ClaimMD (or directly with the payer), and approval is required before eligibility verification can be accessed.
🚀 In most cases, enrollment is Quick Enroll, allowing you to complete it instantly with just one click, no waiting required!
If your agency uses billing integration, you can check client eligibility directly in the system through different sections:
- From the Client’s General List
- When Adding a New Payer to a Client
- In the Eligibility Section
Each of these use cases ensures that you can verify insurance coverage efficiently before providing services.
Checking client Eligibility at the beginning of each month
✅ Monthly Eligibility Check
🔹 Stay ahead! At the beginning of each month, you can verify client eligibility to ensure coverage before scheduling sessions.
🔹 Flexible options: Check eligibility for multiple clients at once or review them individually as needed.
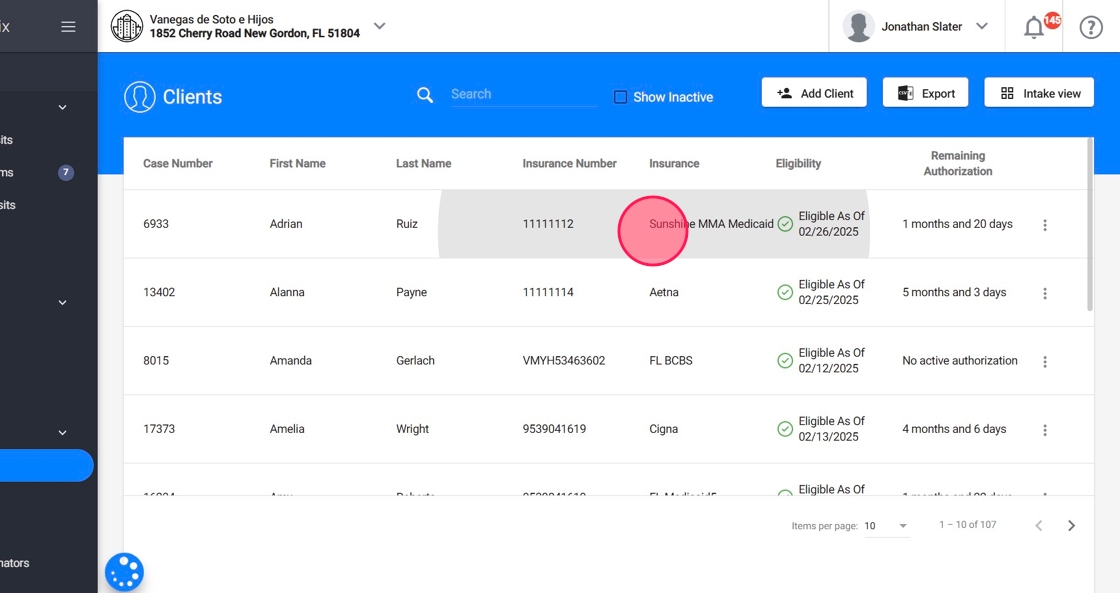
3. Go to the Clients section in the system

4. In this view, you can see:
- Each client’s insurance
- The last recorded eligibility check (e.g., Eligible As Of 02/26/2025).
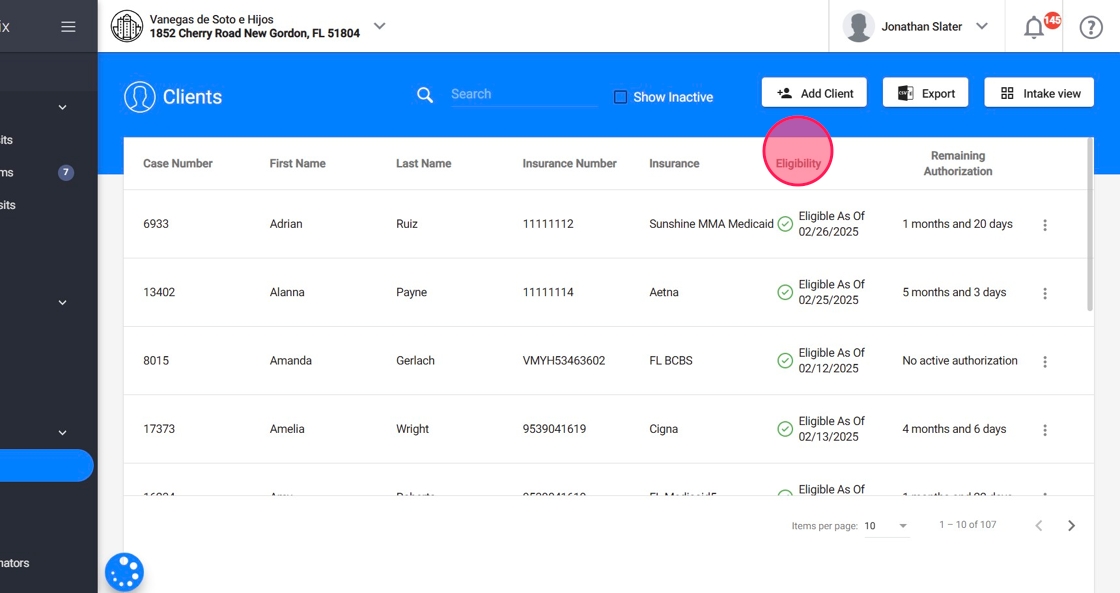
5.✅Eligibility checks for multiple clients:
To run an Eligibility Check for multiple clients just click the option "Run Eligibility"

With this feature, you can quickly check the eligibility of all clients in your agency with a single click at the beginning of each month, making it easy to spot any changes right away
6. Select the date and clients for the eligibility check. Then click Run to initiate the request.

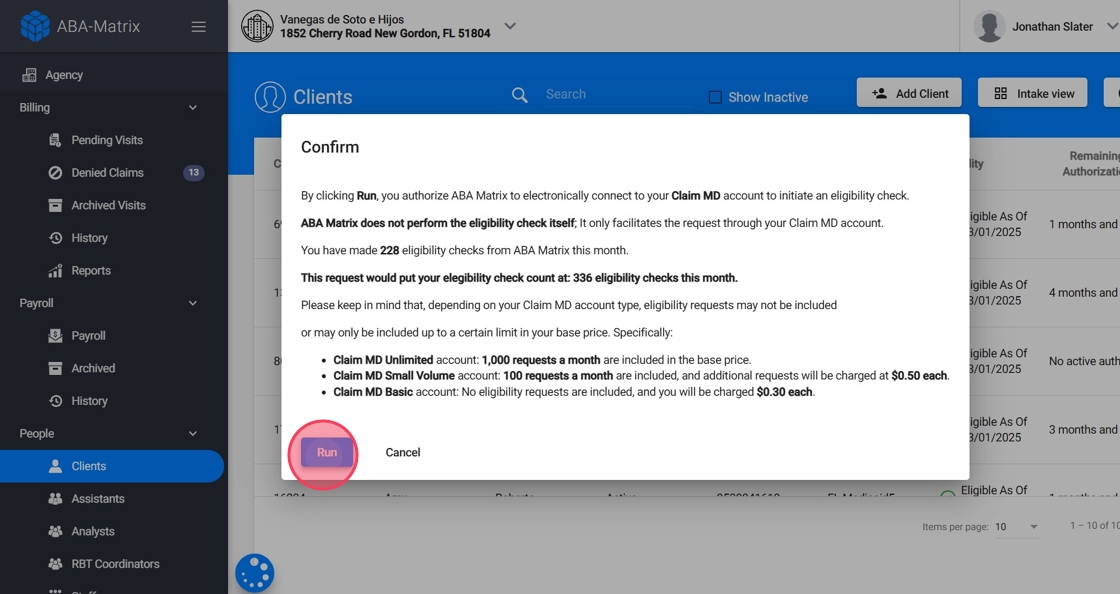
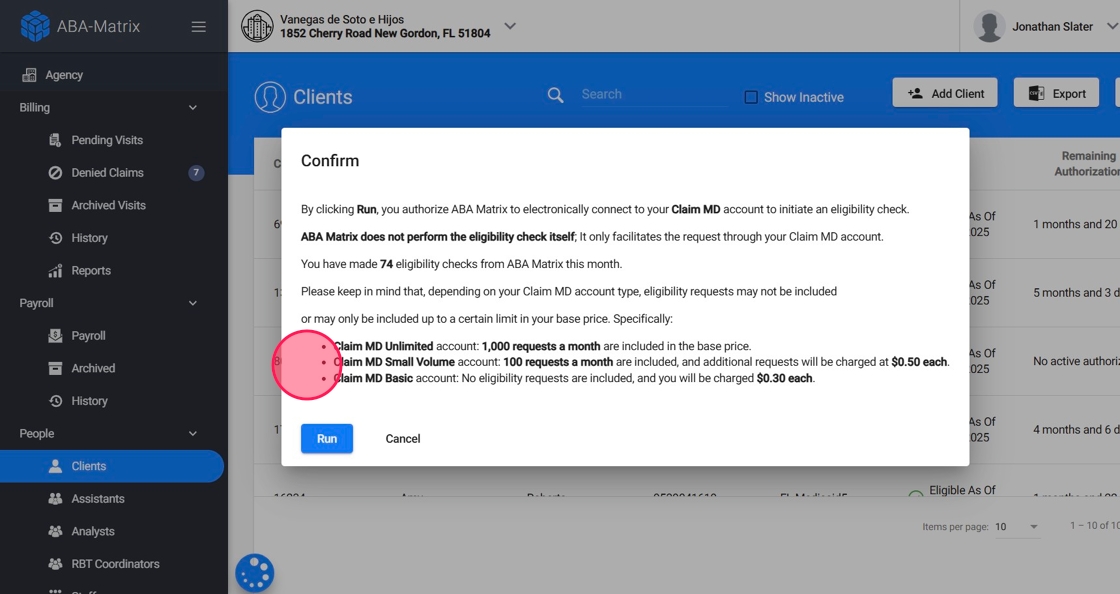
7. Review Eligibility Limits Based on Your Claim MD Plan
A disclaimer will appear:
- “By clicking Run, you authorize ABA Matrix to electronically connect to your Claim MD account to initiate an eligibility check. ABA Matrix does not perform the eligibility check itself; it only facilitates the request through your Claim MD account.”
Below the disclaimer, you will see a summary of how many eligibility checks you have made this month.

Remember that depending on your Claim MD account type, eligibility requests may not be included or may only be included up to a certain limit in your base price:
- Claim MD Unlimited Account: Includes 1,000 eligibility requests per month.
- Claim MD Small Volume Account: Includes 100 eligibility requests per month, with additional requests billed at $0.50 each.
- Claim MD Basic Account: No included eligibility requests; each request is billed at $0.30.
8. Click "Run"
9. The system will verify eligibility and update the client’s record with the latest status.
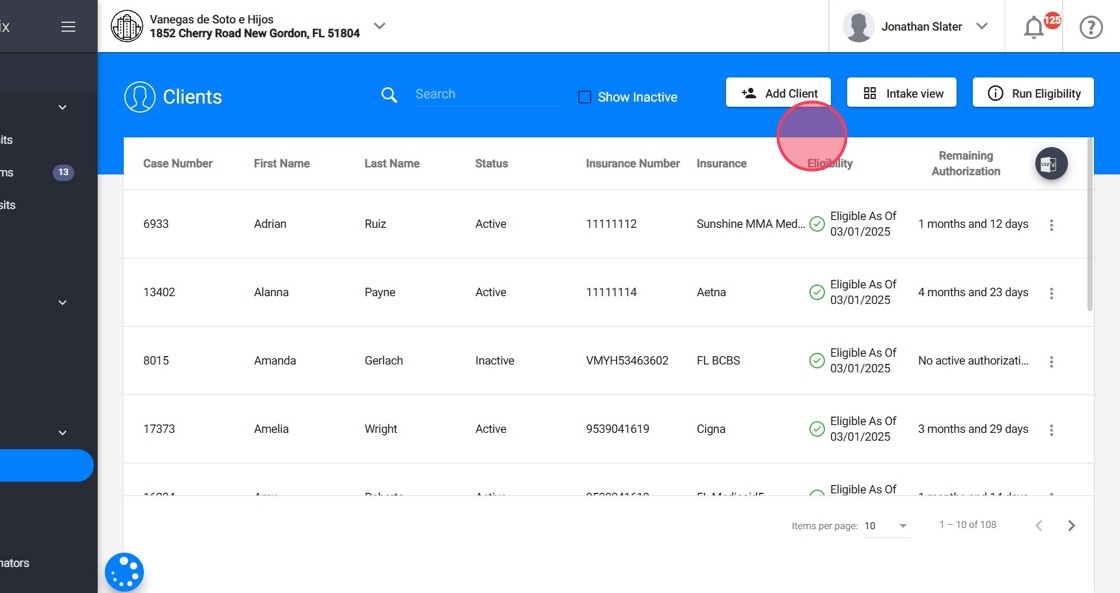
10.✅Eligibility checks for a single client:
To run an Eligibility Check for a single client, click the three-dot menu (⋮) on the right side of the client’s row. Select "Check Eligibility" from the dropdown menu.

11. Review Eligibility Limits Based on Your Claim MD Plan
A disclaimer will appear:
- “By clicking Run, you authorize ABA Matrix to electronically connect to your Claim MD account to initiate an eligibility check. ABA Matrix does not perform the eligibility check itself; it only facilitates the request through your Claim MD account.”
Below the disclaimer, you will see a summary of how many eligibility checks you have made this month.
Remember that depending on your Claim MD account type, eligibility requests may not be included or may only be included up to a certain limit in your base price.
12. Confirm and Check Eligibility:
- Click "Run"
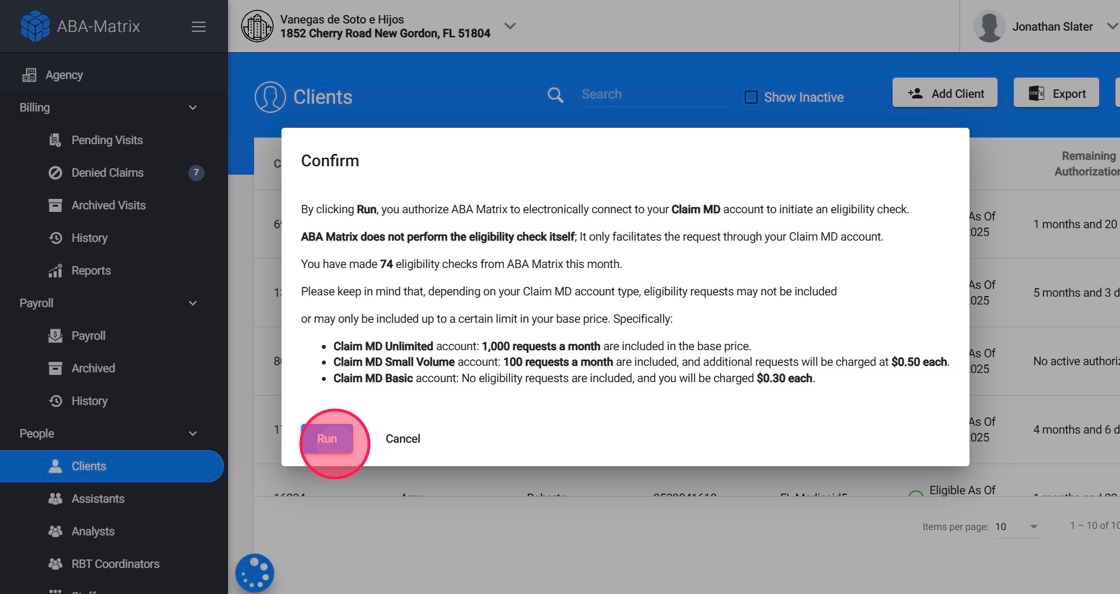
13. Select the date for the eligibility check and click Run to initiate the request.

14. The system will verify eligibility and update the client’s record with the latest status.

15. View Eligibility Details:
Once the check is complete, you can view the EOB (Explanation of Benefits) with all the eligibility details. Just click the three-dot menu (⋮) on the right side of the client’s row and select View EOB from the dropdown menu.
Use this information to confirm coverage before scheduling services for the month.

Checking Eligibility when adding a New Insurance to a client
16. When a client gets new insurance coverage, it’s essential to verify their eligibility before proceeding with billing.
Open the client’s profile.
17. Go to the Insurance section.

18. You can see all the information related to the client's insurances
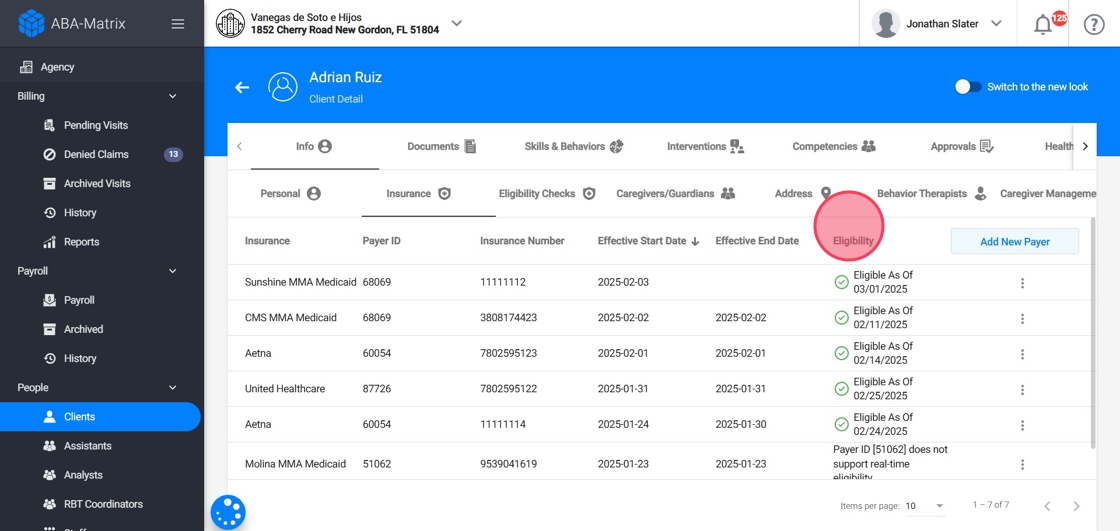
19. Add a New Payer
Click Add New Payer to enter a new insurance provider.

20. Select the insurance provider from the dropdown list.

21. Add the Insurance Number

22. Check Eligibility for the New Payer
- Before finalizing the change, the system will allow you to run an eligibility check.
- Click Check Eligibility to confirm the client’s coverage under the new payer.
- Once eligibility is confirmed, save the new payer details.
- The system will store the verified insurance information, ensuring accurate billing and coverage tracking.

Tracking Eligibility history in the Eligibility Checks section
23. In addition to checking eligibility from the Client’s General List and when adding a New Payer, you can also review a history of all eligibility checks in the Eligibility Section.
Go to the client's Eligibility Checks section

24. Here, you will find a detailed log of all eligibility runs, including:
- The date and time of each eligibility check.
- The client’s insurance status at the time of the check.
- A record of all past eligibility verifications for auditing and reference.
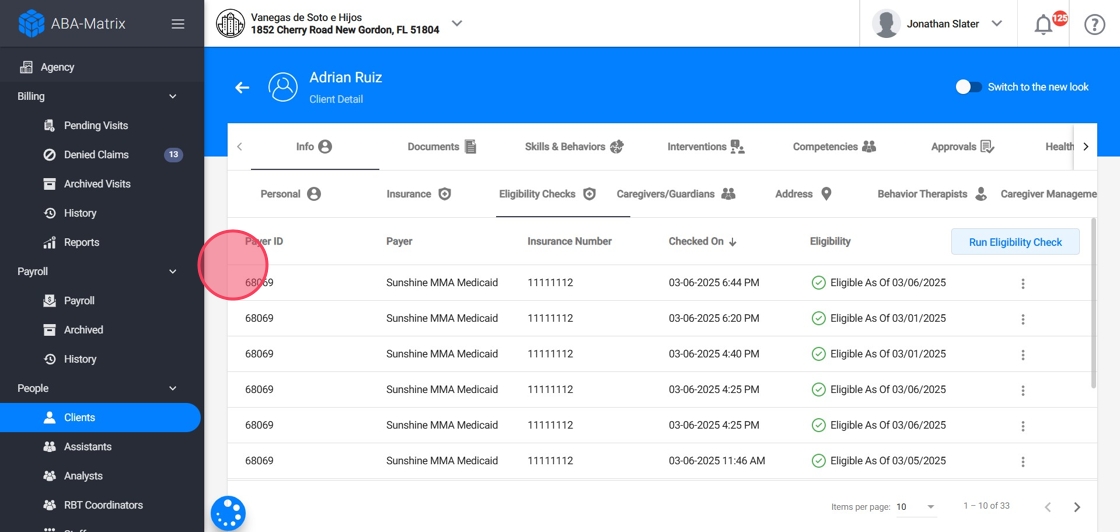
25. You can run Eligibility checks from here as well

This section helps you keep track of coverage updates over time, ensuring accurate billing and reducing potential claim issues.
How to disable the Eligibility Check feature
26. The Eligibility Check feature is enabled by default for agencies using the ClaimMD integration. However, you can disable it at any time through the settings:
- Go to Agency
- Navigate to Settings
- Select Billing Settings
- Disable the Eligibility Checks option
- Click Save

