How to set up the notes system for behavior treatment sessions
The redesigned Behavior Treatment Session Note system is built to support flexibility, clinical accuracy, and alignment with your agency’s unique model of care. As an admin, your configuration choices directly shape the experience of therapists and analysts as they document care, ensuring that every note meets your compliance standards, data collection needs, and clinical style. This guide will walk you through how to set up and manage the global dropdown options used across the new note system.
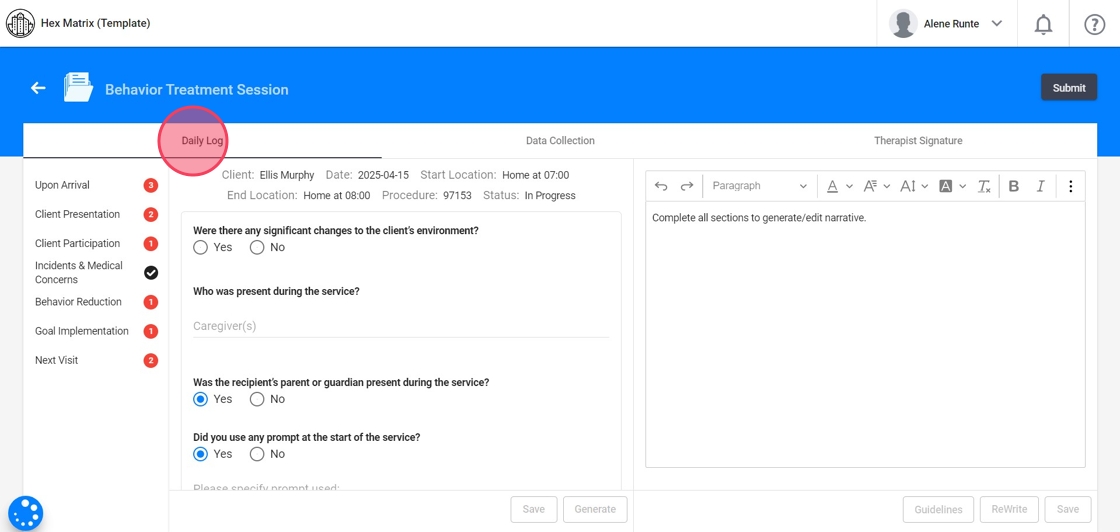
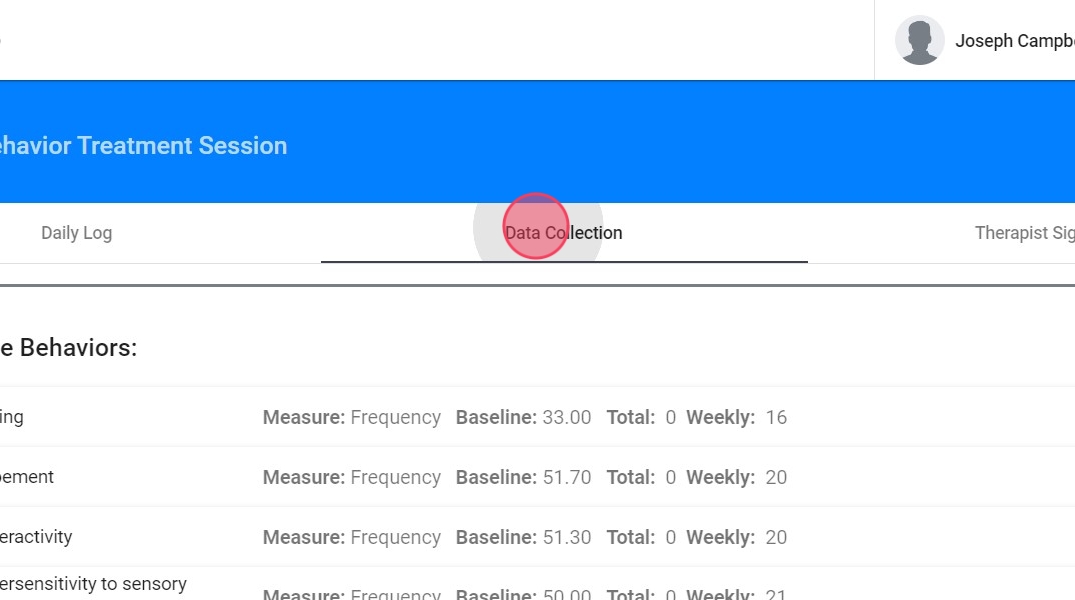
ABA Matrix offers a structured and efficient way to document client session details. The session note is divided into three main sections to support a comprehensive and organized workflow:
- Daily Log: A structured narrative of the session based on specific guiding questions.
- Data Collection: Where you input session data for behaviors, replacement behaviors, and skill acquisition programs. Optional for analysts
- Therapist Signature: The section where the provider signs off on the session note.
1️⃣Configuring Behavior Treatment Notes by Protocol
1. Daily Log: Documenting the Session Narrative
The Daily Log consists of structured questions grouped into sections to ensure that all relevant session details are captured.
When answering questions in the Daily Log, you’ll see suggested prompts you can choose from:
- You can use the suggested prompts as-is
- Edit a selected option to better match the session
- Or type your own response based on what actually occurred during the visit
Always ensure that your final note accurately reflects the session details.
2. Customizable lists for your Agency
Most dropdowns used in the Daily log come from your agency’s configuration, allowing you to control the language, style, and options your team sees. These lists are set up from:
Agency → Forms → Behavior Therapy Session
- Protocol
- Protocol Modification

Index and Alerts
3. At the right side of the note you will have a index for better access to each section within the report. This feature is especially useful for reviewing and editing different parts of the note without having to scroll through the entire document.
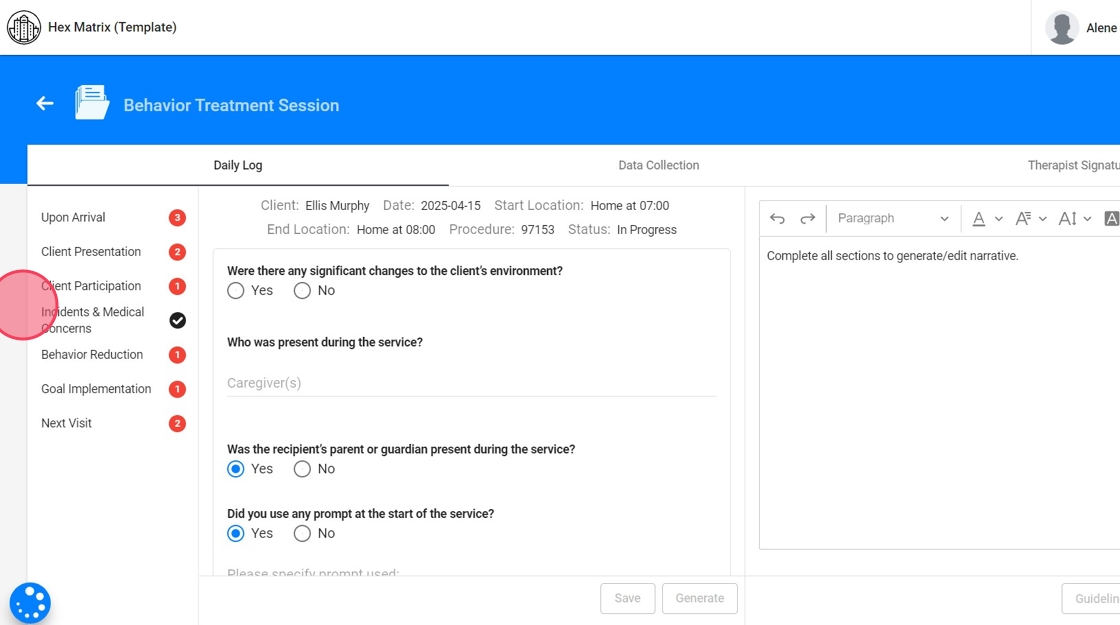
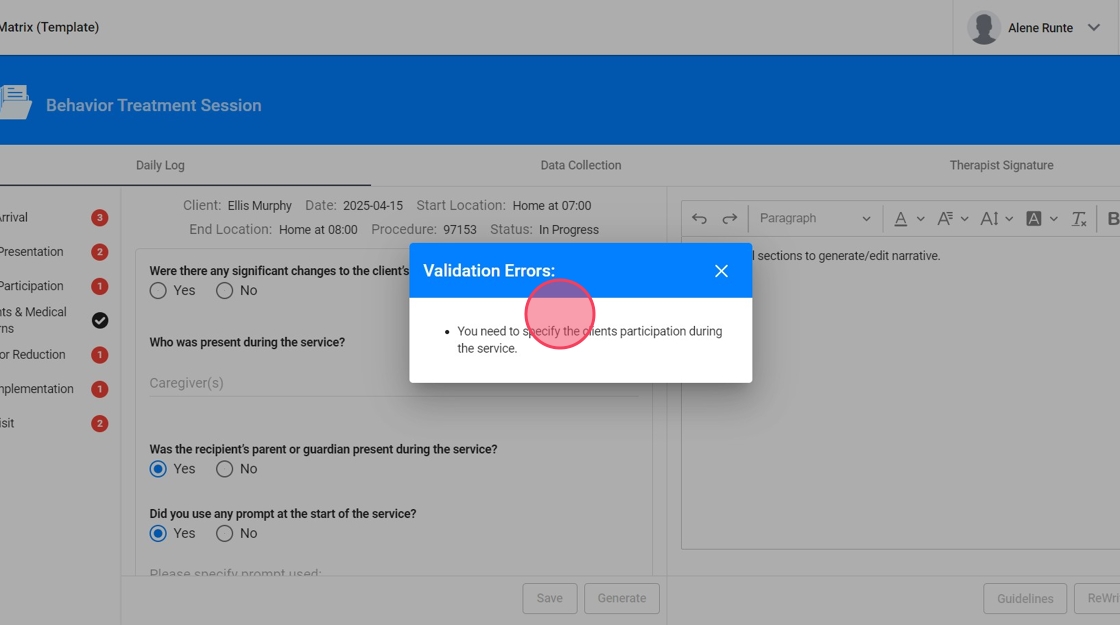
4. - Red alerts:
The red dots with numbers means that specific section has pending work and needs to be edited before submitting the note. The number indicates the amount of pending tasks within the section.
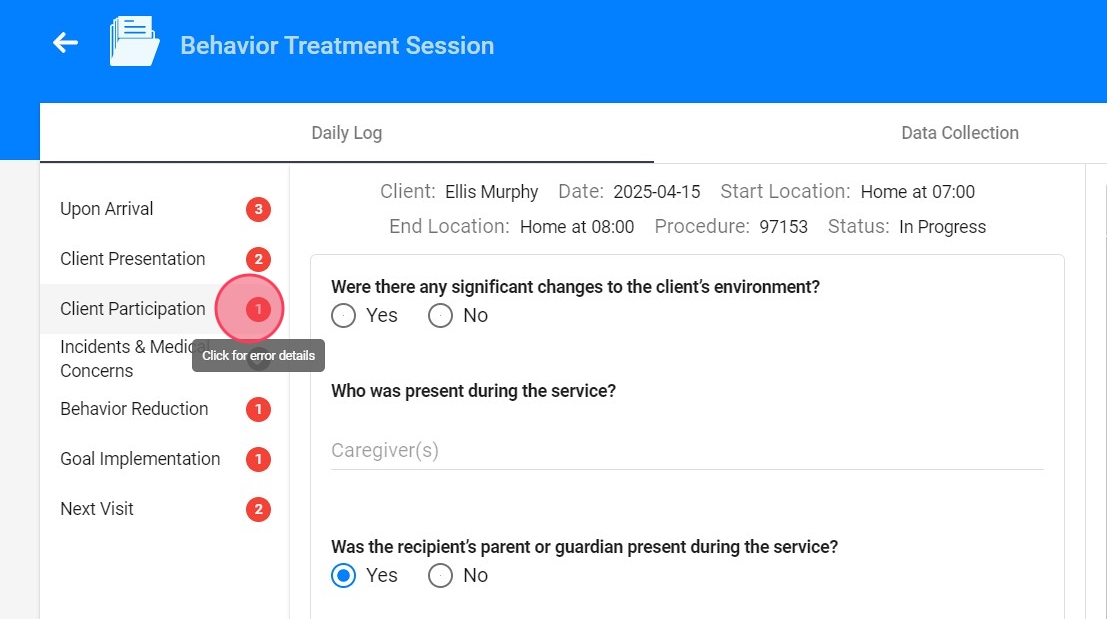
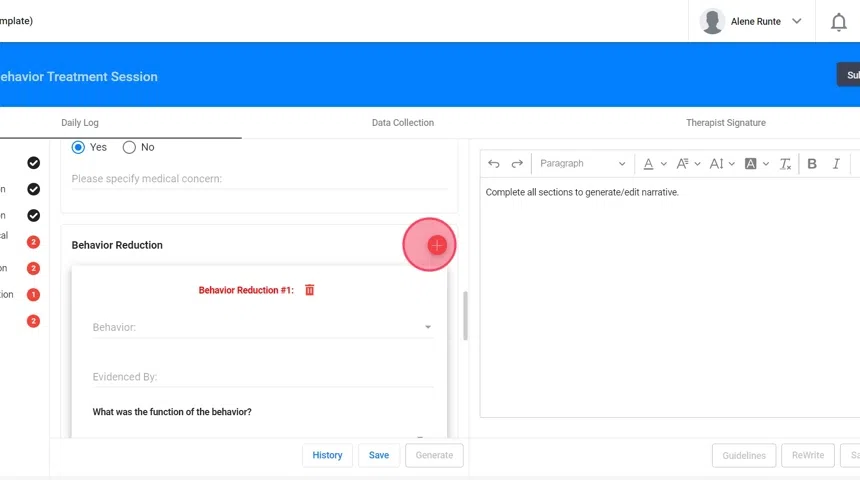
5. Click the alert to see specifically what's missing
Sections of the Note: Upon arrival
6. - Were there any significant changes to the client’s environment? Please select the Environmental Changes.

7. If you select "Yes" in the previous question, a follow-up question will appear: "Were there any manipulations made due to the barriers encountered in the environment?"
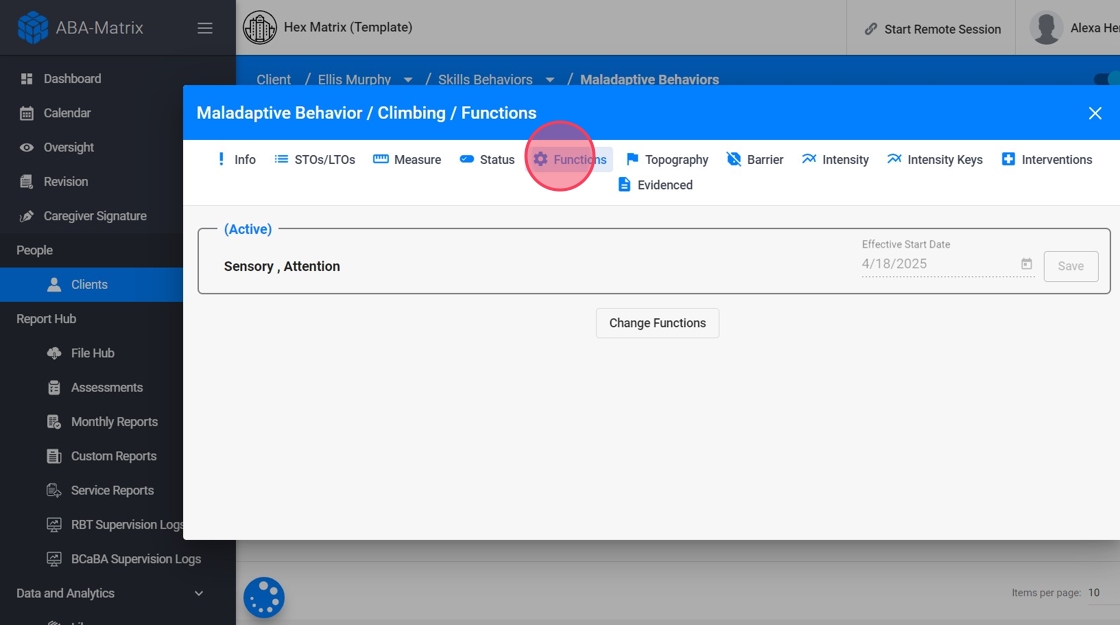
If you select "Yes", you will be asked to select the adjustments you made.

8. Dropdown Customization:
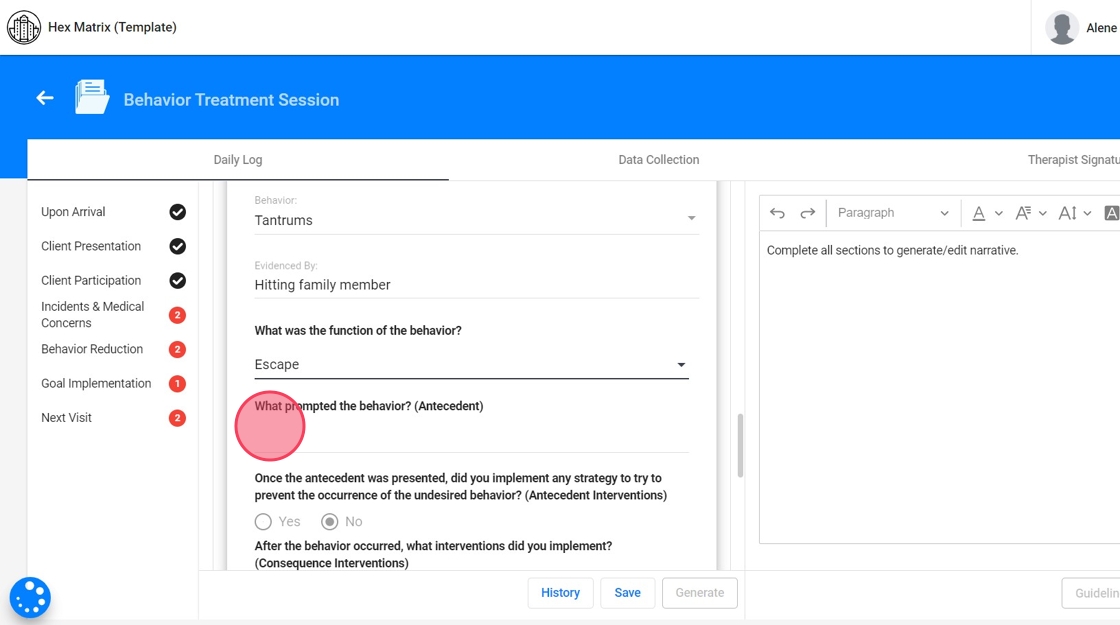
To add or edit options in dropdowns, go to the right of the question and click Configure Lists.

9. You'll see the default options, which you can customize to match your agency's language and workflow. You can:
- Add new options as needed
- Edit the wording of existing options
- Delete any prompts you don’t want to use
These changes ensure that the dropdowns reflect your model of care and guide your team toward consistent, accurate documentation.

10. For Environmental Changes, you can customize both the list of environmental changes and the related manipulations they will see available

11. - Who was present during the service?

12. Dropdown Customization: This information comes from the client’s profile and the caregivers listed there.

13. - Was the recipient’s parent or guardian present during the service? If not, please specify why.

14. Dropdown Customization: To add or edit dropdown options, go to the right of the question and click Configure Lists. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

15. - Did you use any prompt at the start of the service? Please specify the prompt used.
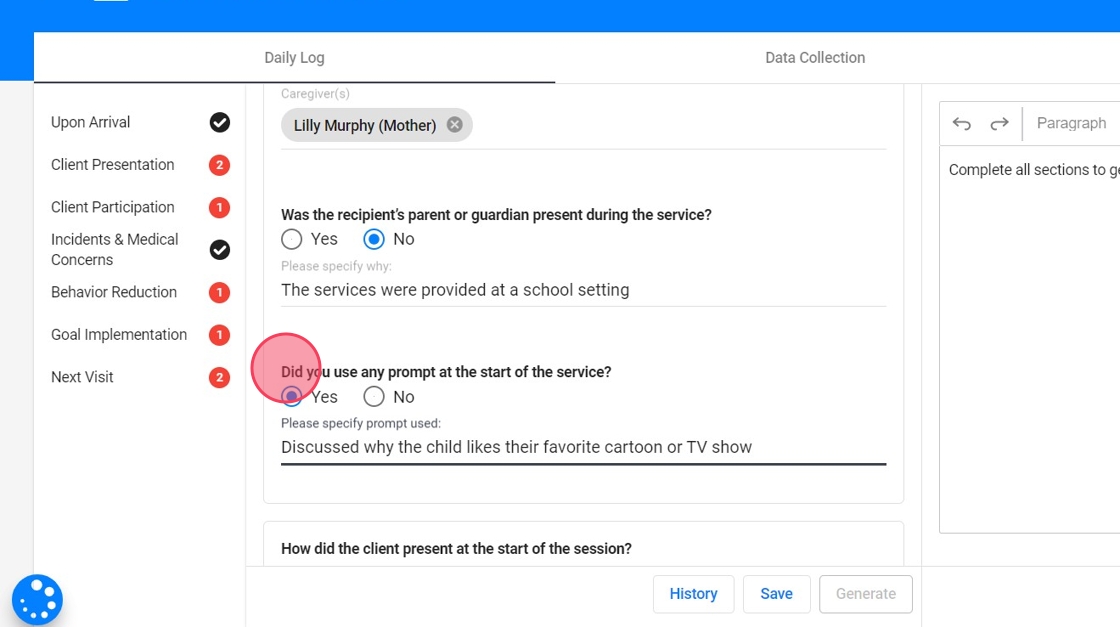
16. Dropdown Customization: To add or edit dropdown options, go to the right of the question and click Configure Lists. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

Sections of the Note: Client Presentation
17. - How did the client present at the start of the session?
- How did the client present at the end of the session?

18. Dropdown Customization: To add or edit dropdown options, go to the right of the question and click Configure Lists. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

Sections of the Note: Client Participation
19. - How was the client's participation during service?

20. Dropdown Customization: To add or edit dropdown options, go to the right of the question and click Configure Lists. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

Sections of the Note: Incidents and Medical Concerns
21. - Were there any incidents during the service? If you select "Yes", please specify the incident.
- Were there any medical concerns? If you select "Yes", please specify the concern.

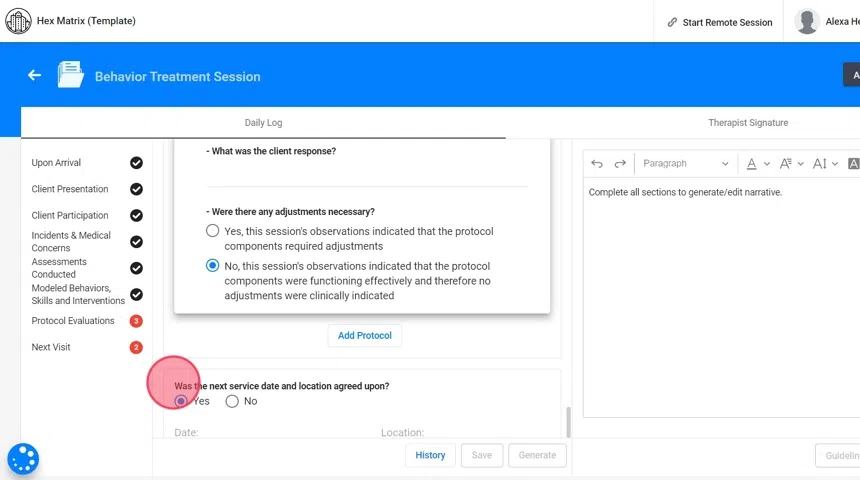
22. Dropdown Customization: To add dropdown options, go to the right of each question and click Configure Lists. From there, you can add the information as needed.

Sections of the Note: Behavior Reduction
23. In this section, you will see a drop-down list showing all the client's behaviors that are active at the time of the session.
Select the behavior that is being targeted for reduction.
24. For each behavior you select, you will complete an Evidence By section.

25. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

26. Some fields pull directly from the client’s profile. In this case, you can use prompts from the profile and tailor the information to the specific behavior being addressed.
- Go to the Behaviors section of the client profile.
- Under each behavior, you'll find an area labeled "Evidence-by Options" where you can define how that behavior typically presents
- These options will appear in the RBT’s dropdown when documenting behavior reduction.

27. - What was the function of the behavior? Select one of the functions that has been set up for the selected behavior.

28. Dropdown Customization directly in the client's profile:
- Go to the Behaviors section of the client profile.
- Under each behavior, you'll find an area labeled "Functions"
- These functions will appear in the RBT’s dropdown when documenting behavior reduction.
29. - What prompted the behavior? (Antecedent)? You’ll see a list of potential antecedents that correspond to that function.
30. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. The list of antecedents is directly linked to the selected function of the behavior. You can adjust this list as needed: add new options, edit existing ones, or remove any that don’t align with your model of care.

31. - Once the antecedent was presented, did you implement any strategy to try to prevent the occurrence of the undesired behavior? (Antecedent Interventions)
A list of available antecedent interventions will appear, tailored to the selected behavior.
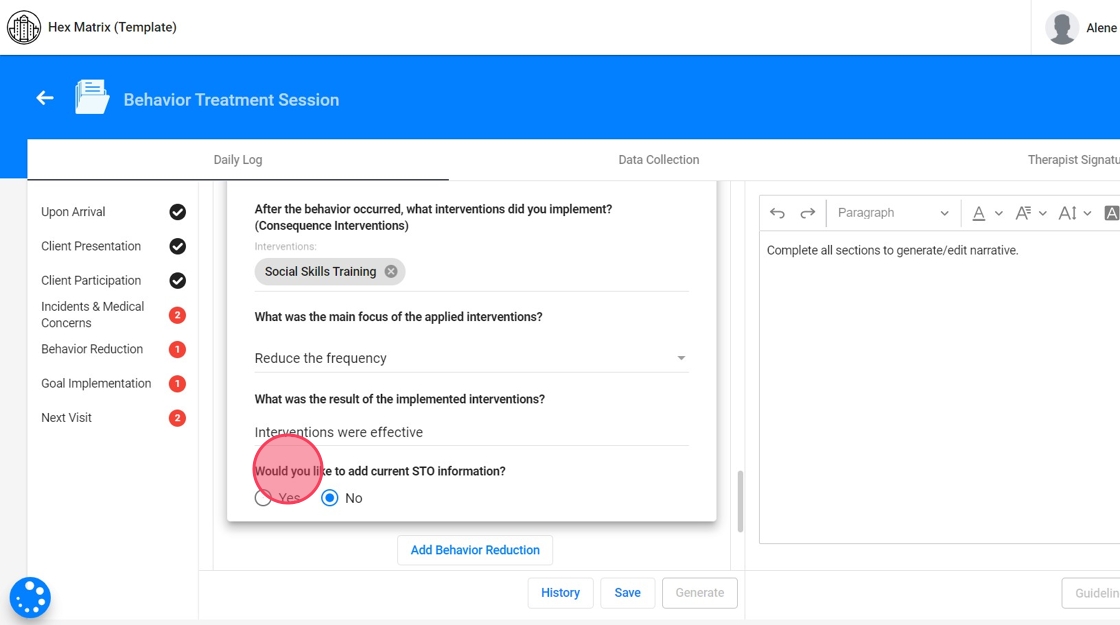
- After the behavior occurred, what interventions did you implement? (Consequence Interventions)
Based on the selected behavior, a list of consequence-based interventions will appear for you to select from.

32. Dropdown Customization directly in the client's profile:
- Start in the Interventions section of the client profile.
- First, categorize each intervention as either Antecedent or Consequence-Based.
- Once interventions are classified, go to the Behaviors section, select a behavior, and link the appropriate antecedent and consequence interventions to that behavior.
These options will appear in the RBT’s note as dropdowns when documenting behavior reduction, tailored to the selected behavior.

33. - What was the main focus of the applied interventions?
These options depend on the selected behavior measurement. For example, if the measurement of the behavior is frequency, then the system will default to “Reduce the frequency.” You can always select “Other”, and manually enter a focus that better aligns with the client’s specific needs.

34. - What was the result of the implemented interventions?
35. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

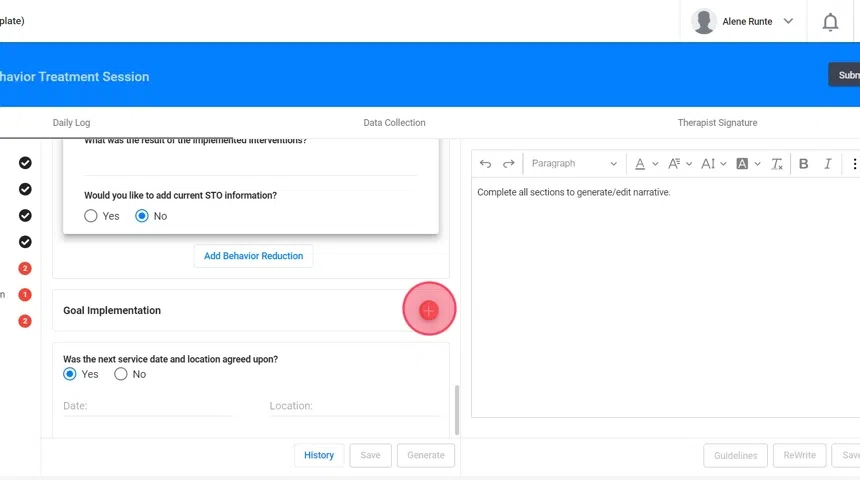
36. - Would you like to add current STO information? If you select "Yes" the system will include this information in the narrative
Sections of the Note: Goal Implementation
37. In this section, you will see a drop-down list showing all the client's programs that are active at the time of the session.
Select the implemented program you wish to describe.
38. - What activities were used for implementation?

39. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

40. - What was the teaching procedure used? The available options come from the selected program's information in the client’s profile

41. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

42. In this case, you can tailor the information to the specific program and pull prompts directly from the client’s profile.
Dropdown Customization directly in the client's profile:
- Go to the Programs tab in the client profile.
- For each active program, define the teaching procedures
- These will populate the dropdown based on the selected program in the RBT note.

43. - Did you use any prompts? If you select "Yes", select the prompt

44. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

45. - What reinforcers were used? Select the reinforcers that were used to support goal implementation

46. In this case, you can tailor the information to the specific client and pull prompts directly from each profile.
Dropdown Customization directly in the client's profile:
- In the client profile, go to the Preferences section.
- Add reinforcers the client currently responds to (e.g., iPad, snacks, praise).
- These populate the dropdown when RBTs report what was used during session.

47. You can always set up a general list of preferences for the agency. If a client’s individual preferences haven’t been configured yet, the system will use the agency-wide list as the default for the reinforcers section of the note.

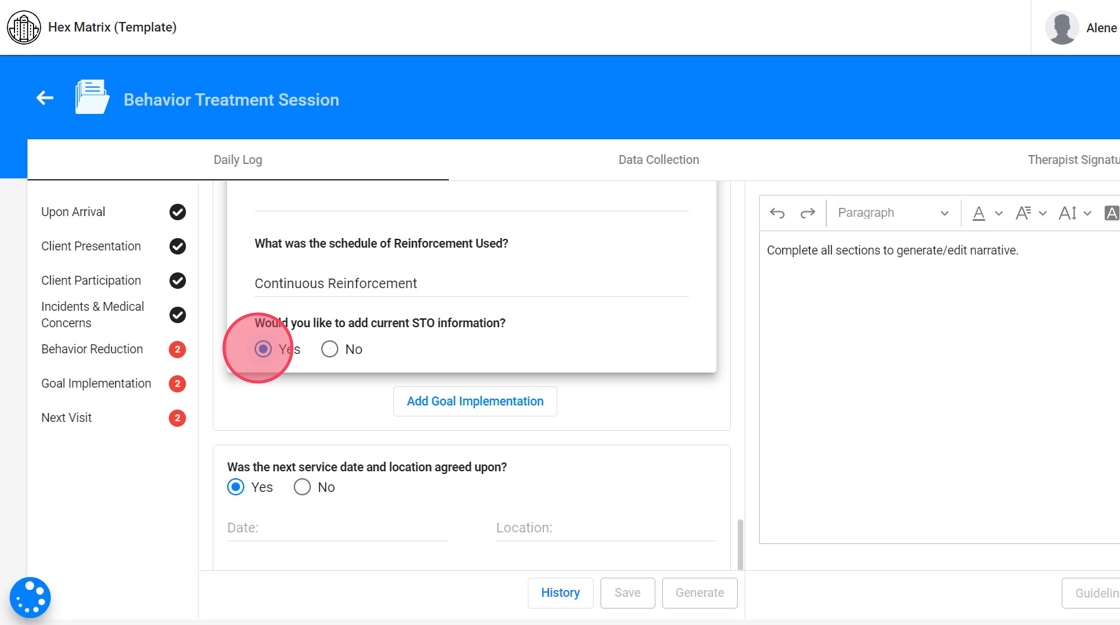
48. - What was the schedule of Reinforcement Used?

49. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit. From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.

50. In this case, you can tailor the information to the specific program and pull prompts directly from the client’s profile.
Dropdown Customization directly in the client's profile:
- In the client’s Program, define the schedule of reinforcement.
- These appear as selectable options in the note when documenting program implementation

51. - Would you like to add current STO information? If you select "Yes" the system will include this information in the narrative
Sections of the Note: Next Visit
52. - Was the next service date and location agreed upon?
- If so, specify the Date and Location.
- If not, specify why the next service date and location was not agreed upon.

Generate narrative
53. Once you've filled out the sections of the note, clicking the "Generate" button will prompt the system to compile the data you’ve entered. The AI takes all the responses and selections made across different sections and synthesizes them into a coherent progress narrative.

54. The generated narrative is presented as an editable draft. You can review the narrative, make any necessary adjustments, and ensure that it accurately reflects the session's details before finalizing the note.

Guidelines Integration
55. The system includes predefined guidelines that ensure the progress note meets the standards required.

56. After generating the progress note, the AI will analyze the content to determine whether it complies with the established guidelines.
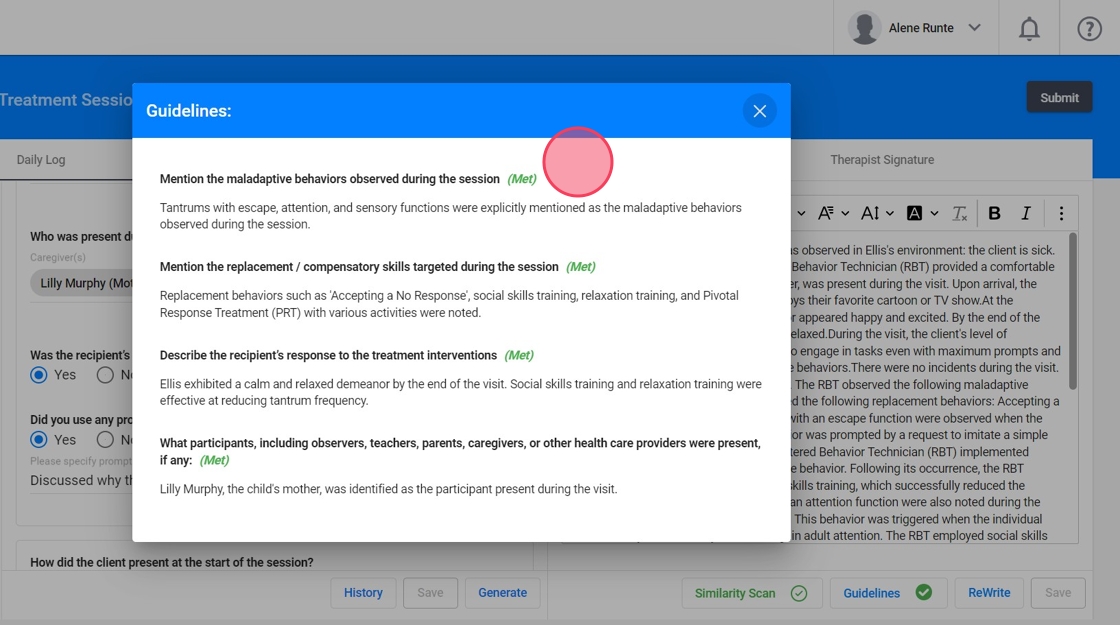
These guidelines are defined by your agency and can be customized for each payer or insurance provider.
They will also be visible from Oversight, Revision, and Quality Assurance.
Similarity scan
57. When the narrative is generated, automatically runs a Similarity Check in the background to ensure notes are not overly repetitive.
- This step happens in real time while the narrative is being generated.
- The system compares the content of your current note with previous entries, checking for similarity based on the percentage allowed by the agency.

58. You can define an allowable percentage of similarity and set up the system to prevent users from submitting notes that are similar.
Just go to Settings → Daily Log and enable the features.

59. If a note exceeds the allowed similarity threshold, the system will prompt you to revise it before submission. A similarity report will be generated, comparing your current note to previous ones. It highlights overlapping text in red and differences in green, helping you spot areas that need revision.
To resolve issues:
- Review the highlighted text for concerns
- Edit the “Current Progress” to make content unique
- Save and recheck until the note falls within the agency’s acceptable similarity range

History
60. Every time you click "Save" or "Generate Progress," the system automatically takes a snapshot of the note in its current state. This snapshot serves as a version of the note that you can recover at any time in the future.
You can open any snapshot to review the content as it was at that specific moment. This is particularly useful if you need to verify details, compare different versions, or understand the progression of the documentation process.

Data collection
61. When collecting data for behaviors, replacements, or skills, the way you select and manage these entries affects how they are represented in the system’s graphs.
62. If you do not select a specific behavior, replacement, or skill for data collection, that item will not appear in the generated graph.

63. If you choose to mark a behavior, replacement, or skill for data collection but do not input any data for it, the system will automatically record a value of 0 for that session.

2️⃣ Configuring analysts notes for Protocol Modification
64. All prompts for the fields in the Analyst’s Notes come directly from your agency’s form configuration. These fields are fully customizable in the same way as the Protocol section, by clicking Configure Lists next to each field within the form builder.
This ensures consistency across documentation and allows you to tailor the prompts to your agency’s clinical standards and workflows.

65. Daily Log: Documenting the Session Narrative
The Daily Log consists of structured questions grouped into sections to ensure that all relevant session details are captured.

Sections of the Note: Upon arrival
66. - Were there any significant changes to the client’s environment?
- You can select the environmental change and add it to the client’s data graph by checking the option “Add Environmental Changes on this date to graphs". If you indicate “Yes”, a follow-up question will ask whether any manipulations were made in response and select the specific adjustments implemented.
- Who was present during the service?
- Was the recipient’s parent or guardian present during the service?
- If not, please specify why.
- Did you use any prompt at the start of the service? Please specify the prompt used.
- Deficits or barriers identified for remediation during the visit

Sections of the Note: Client Presentation
67. - How did the client present at the start of the session?
- How did the client present at the end of the session?

Sections of the Note: Client Participation
68. - How was the client's participation during service?

Sections of the Note: Incidents and Medical Concerns
69. - Were there any incidents during the service? If you select "Yes", please specify the incident.
- Were there any medical concerns? If you select "Yes", please specify the concern.
You can add these incidents and/or medical concerns to the graph directly from the note.

Sections of the Note: Assessments Conducted
70. - Were there any Assessments Conducted? If you select "Yes", you must select the Assessment conducted and explain it. You can add the assessment to the graph directly from the note.

71. Dropdown Customization: To add or edit dropdown options, go to the right of the question and click Configure Lists. From there, you can adjust the information as needed: add new options and preset explanations for the selected assessments, edit existing ones, or remove any that don’t apply to your model of care.

Sections of the Note: Modeled Behaviors, Skills and Interventions
72. - Did you observe or redirect any behavior during the visit?
- Did you model any intervention during the visit?
- Did you model any replacement during the visit?
You must select and explain your selections

Sections of the Note: Protocol Evaluations
73. To add a protocol evaluation, click the red + sign and select what was targeted (e.g., maladaptive behavior, replacement, skill, intervention, or other). Based on your choice, specific questions and prompts will appear.
You’ll need to indicate whether you're working on an existing or new item. For existing items, a list from the client’s profile will appear for selection.
You’ll then be asked:
-
Whether a plan component was evaluated. If yes, specify what was evaluated and whether any adjustments were needed, with explanations.
Whether an active direction was given to the technician. If yes, describe the direction provided.
Whether a specific protocol was implemented. If yes, you’ll need to provide:
- The objective of implementation
- The protocols used
- The client's response
- Any necessary adjustments, with explanations

74. Dropdown Customization: To add or edit dropdown options, go to the right of the question, click Configure Lists and select the field you want to edit:
- Plan Components
- Active Directions Given To RBT
- Objectives of the Implementation
- Implemented Protocols
- Client Responses
From there, you can adjust the information as needed: add new options, edit existing ones, or remove any that don’t apply to your model of care.
Sections of the Note: Next Visit
75. - Was the next service date and location agreed upon?
- If so, specify the Date and Location.
- If not, specify why.
Generate narrative
76. After completing the note sections, click “Generate” to have the system automatically compile your inputs into a progress narrative. The AI will use your responses and selections to create a coherent draft, which you can then review, edit, and finalize to ensure it accurately reflects the session.

Similarity scan
77. When the narrative is generated, the system automatically performs a real-time Similarity Check to ensure notes are not overly repetitive. It compares your current note against previous entries, based on the similarity threshold set by your agency.
If the note exceeds that threshold, you’ll be prompted to revise before submitting. A detailed Similarity Report will show:
-
Current progress (your note in progress)
Previous progress (notes it’s being compared to)
Comparison highlights:
- Red = similar content
- Green = differing content
To resolve concerns:
- Review the highlighted text
- Edit the "Current progress" section as needed—changes update the comparison in real time
- Repeat the check until the note meets the required uniqueness level

History
78. Each time you click “Save” or “Generate Progress,” the system automatically creates a snapshot, a version of the note at that moment. All snapshots are saved with the date and time, allowing you to:
- Track how the note evolved over time
- Compare different versions
- Verify or recover previous content as needed
You can open any snapshot to review the note exactly as it was when saved.

Admins have full control over the content and structure of the new Behavior Treatment Session Notes. Here's what you can configure:
-
General Dropdowns & Terminology:
Customize all standard fields and terminology used in the notes from Agency → Forms → Behavior Treatment Session Form.
-
Tailor the language and available selections for each field to match your agency’s model of care.
Behavior & Program-Specific Prompts:
These are pulled directly from client profiles, ensuring relevance and accuracy.
- Behavior Reduction Sections: Pulls directly from each behavior the evidence list, identified functions, and selected antecedent and consequence-based interventions.
- Goal Implementation Sections: Pulls from each program’s configuration teaching methods and reinforcement schedules, as well as reinforcers from the client’s preference list.
